Modifying Lifestyle to Improve Breast Cancer Survivorship

Modifying Lifestyle to Improve Breast Cancer Survivorship
As per WHO reports, in 2020, there were approximately 2.3 million women diagnosed with breast cancer and 685,000 deaths globally.1 Numerous evidence-based studies have suggested that weight management and increased physical activity are important in breast cancer prevention and control. Observational studies have demonstrated that obesity can increase the risk of breast cancer recurrence and mortality in pre- as well as postmenopausal women. Evidence also suggests that inactivity, irrespective of its contribution to adiposity, can trigger breast cancer incidence and mortality. Despite the evidence that links obesity and inactivity to breast cancer, much less has been explored on the impact of weight loss or physical activity in lowering the risk of breast cancer. Moreover, these lifestyle changes have the potential to improve outcomes in individuals who are diagnosed with early-stage cancer that is potentially curable.
Obesity and lifestyle - impact on breast cancer risk and prevention
Much evidence has demonstrated that BMI is linked to an increased risk of postmenopausal breast cancer unlike in premenopausal breast cancer where higher BMI is associated with a reduced risk.
Obesity increases the risk of developing postmenopausal breast cancer by 1.5 to 2 times. For every 5 kg gain in body weight above the lowest adult weight, there has been an estimated increase in the postmenopausal breast cancer risk by 4% to 8%. Postmenopausal women with excess adiposity are known to have an increased risk of estrogen receptor-positive (ER+) and progesterone receptor-positive (PR+) breast cancers.
This risk is limited or stronger in individuals who have not used hormonal therapy (HT). Weight gain has been more strongly related to ER+ and PR+ than to ER− and PR− tumors. Metabolic dysfunction, inflammation, and production of postmenopausal estrogen are known to increase adiposity, specifically visceral adipose tissue.
Weight fluctuations or weight cycling occurs in overweight and obese women when intentional weight loss is not maintained. However, deleterious changes in the body such as increased fat, decreased lean mass, and deposition of preferential abdominal fat with aging can be masked by a stable BMI. The insufficient precision of BMI for adipose estimation with aging probably plays a role in the differential pre- and postmenopausal relation in breast cancer and obesity. Thus, it is important to consider accurate direct measures of body composition such as dual-energy x-ray absorptiometry. Metabolic dysfunction, chronic low-grade inflammation, metabolic syndrome, and type 2 diabetes accompanied by obesity are considered important risk factors for developing postmenopausal breast cancer. In addition, type 2 diabetes alone without BMI is associated with an increased risk of breast cancer.
Screening via mammography is routinely practiced in breast cancer detection; high mammographic density is linked with breast cancer. Higher levels of physical activity might reduce the risk of breast cancer. Studies have shown that the relationship between physical activity and breast cancer is independent of BMI, ER status, weight gain, and HT. Vigorous physical activities, walking, and household chores can reduce the risk of breast cancer in pre- as well as postmenopausal women. These physical activities associated with breast cancer risk are independent of smoking status and have shown a significant delay in the onset of breast cancer among carriers of BRCA. Physical activity helps in reducing the risk of developing breast cancer by lowering the estrogen availability, inflammation, and metabolic dysfunction along with an improvement in body composition. Figure 1 represents cancer prevention guidelines and their impact on breast cancer risk.
Figure 1:Cancer prevention guidelines and their impact on breast cancer risk.
Compiled guidelines from World Cancer Research Fund/American Institute for Cancer Research (2018) And American Cancer Society (2012)
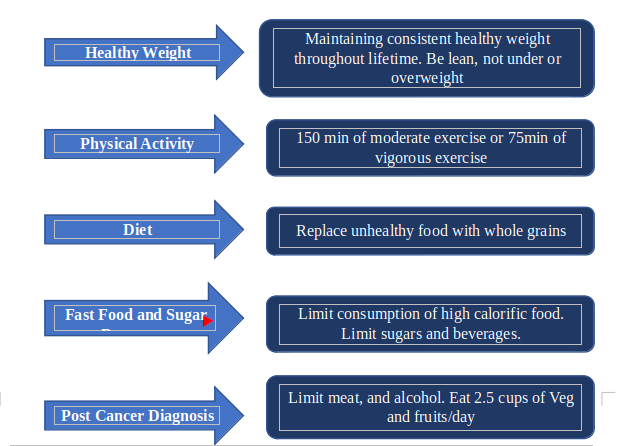
Figure 2 represents the American Cancer Society Guidelines on nutrition and physical activity for cancer survivors.
Figure 2: American Cancer Society Guidelines on nutrition and physical activity for cancer survivors.
Breast cancer survivorship - the impact of weight, physical activity, and diet
An earlier meta-analysis of data from 213,075 women with early-stage breast cancer study reported a 35% increase in breast cancer-related mortality and a 41% increase in overall mortality in obese women versus normal BMI women diagnosed with breast cancer. Obese premenopausal women had a 75% increased risk of mortality postdiagnosis, whereas normal weight premenopausal women and obese postmenopausal women had a 34% increased risk of mortality after cancer diagnosis. Another study reported that high levels of physical activity after a cancer diagnosis reduced the risk by 29% for breast cancer-specific mortality and a 43% for all-cause mortality in survivors who were physically active post cancer diagnosis.
Post diagnosis lifestyle change - recurrence and mortality
There is now substantial evidence demonstrating the relationship between breast cancer outcomes and the dietary patterns of women. In the Women’s Intervention Nutrition Study conducted on 2437 women with Stages I to III breast cancer, at least a 20% reduction of daily calories from fat to a low-fat dietary intervention significantly improved the disease-free survival. An exploratory subgroup analysis further revealed that a significant survival benefit was observed in patients with ER− breast cancer. Another similar study (The Women’s Healthy Eating and Living study) conducted on 3088 women with Stages I to III breast cancer demonstrated dietary intervention (increasing the intake of fruits, vegetables, and fibers and lowering fat intake) did not aid in weight loss and no difference in recurrence rates between the diet and control groups (16.7% vs. 16.9%; p = 0.63). Several other studies including SUCCESS-C Trial DIANA-5 (Mediterranean diet) and Breast cancer Weight Loss (BWEL) studies further suggest a calorie-restricted, low-fat diet with increased physical activity in patients improves the disease-free and overall survival. Based on these evidences, the American Cancer Society provides guidelines on nutrition and physical activity for cancer survivors (Figure 2).
Yet, there are challenges to incorporate all of these components in the survivorship care program. These can be implemented successfully by adequate patient education and awareness followed by counseling and referral of patients to appropriate programs that in turn can help them to perform the right exercises and physical activities and track them.
Figure 3 represents the effective execution and implementation of physical activity and weight management interventions in survivorship care.
Figure 3:Physical activity and weight management interventions in survivorship care.
To conclude, physical exercise and weight management benefit breast cancer survivors by improving cardiovascular respiratory fitness, reduction in fatigue, physical fitness, reducing anxiety and depression, and improvements in metabolic and inflammatory biomarkers. There is an unmet need for establishing best practices to incorporate these dietary interventions and physical activities in the survivorship care program and share more success stories.
References:
- https://www.who.int/news-room/fact-sheets/detail/breast-cancer
- Ligibel JA et al. Weight management and physical activity for breast cancer prevention and control. Am Soc Clin Oncol Educ Book. 2019;39:e22–e33.
Disclaimer: The Views/Opinions expressed and/or opinions provided in Videos and other content on MedEnrich Website are those of respective speakers. They do not purport to reflect the opinion or views of Dr.Reddy’s Laboratories Limited or its affiliates (collectively Dr.Reddy’s)in any manner whatsoever and accordingly ,Dr.Reddys does not recommend , endorse or make any representation about the veracity and appropriateness of the views ,opinions/ information on MedEnrich website. Content on MedEnrich website may discuss uses and dosage for therapeutic product that may not have been approved in by the relevant regulatory agencies in your country. Dr.Reddy’s does not support , endorse or encourage any off-label use. Please refer to approved label before prescribing.